General medicine case discussion
This is an E log book to discuss our patient's de-identified health data shared after taking his guardian's signed informed consent. Here we discuss our individual patient problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable comments in comment box are most welcomed
I have been given this case to solve in an attempt to understand the topic of "Patient clinical data analysis" to develop my competency i reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
K. Tejarshini (Intern)
42Year old male presented with complaints of,
Abdominal pain since 4 Days
Decreased urine output since 4 Days
Constipation since 4 Days
Vomitings since 4 Days
History of presenting illness:
Patient was apparently asymptomatic 4 Days back then he complained of abdominal pain which is diffuse associated with vomitings which is bilious, non-projectile, greenish in color, associated with constipation, passed stools 3Days back.
Patient also complained of decreased urine output since 3Days.
There is a history of continuous alcohol consumption since 10 Days without intake of food.
Stiffness of joints yesterday night.
No loss of consciousness, giddiness, fever.
Past History:
Not a Known case of DM, HTN, Asthma, Epilepsy, CAD, CVA.
30/12/22:
Soap notes
AMC
Bed no:5
UNIT-3
Dr. Nikitha (SR)
Dr. Vamshi (Pgy3)
Dr. Nishitha (Pgy2)
Dr. Govardhini (Pgy1)
S:
Stools passed
No Fever spikes
O:
Temp- Afebrile
Bp-110/70mm hg
Pr- 70bpm
Rr-16cpm
Spo2- 99% on RA
GRBS:112mg/dl
I/O charting:2400/950ml
Systemic Examination:
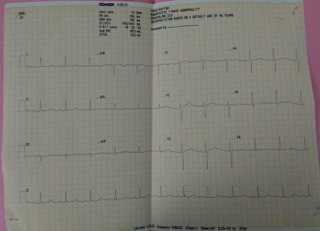
Cardiovascular System : S1, S2 heard, no
murmurs
Respiratory System : Bilateral air entry present.Normal vesicular breath sounds heard.Position of trachea central.
Central Nervous System : patient is conscious coherent and cooperative. Higher mental functions intact
Per abdomen : soft, non tender. No organomegaly.
A:
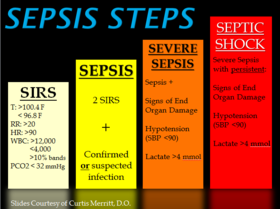
SIRS (Resolved)with MODS-Thrombocytopenia, ALI(Resolving),AKI(Resolved),HYPOKALEMIA(RESOLVED) , HYPONATREMIA(RESOLVED).
DCMP-SEPTIC /ALCOHOL INDUCED.
P:
IVF 2 units-2unitsNS, 1Unit RL@75ml/hr
Inj. DOXY 100mg iv/BD
Inj. THAIMINE 200mg in 100ml NS iv/BD
SYP. LACTULOSE 15ml HS
31/12/23:
Soap notes
AMC
Bed no:5
UNIT-3
Dr. Nikitha (SR)
Dr. Vamshi (Pgy3)
Dr. Nishitha (Pgy2)
Dr. Govardhini (Pgy1)
S:
Stools passed
No Fever spikes
O:
Temp- Afebrile
Bp-120/70mm hg
Pr- 80bpm
Rr-19cpm
Spo2- 99% on RA
GRBS:115mg/dl
I/O charting:2000/900ml
Systemic Examination:
Cardiovascular System : S1, S2 heard, no
murmurs
Respiratory System : Bilateral air entry present.Normal vesicular breath sounds heard.Position of trachea central.
Central Nervous System : patient is conscious coherent and cooperative. Higher mental functions intact
Per abdomen : soft, non tender. No organomegaly.
A:
SIRS (Resolved)with MODS-Thrombocytopenia, ALI(Resolving),AKI(Resolved),HYPOKALEMIA(RESOLVED) , HYPONATREMIA(RESOLVED).
DCMP-SEPTIC /ALCOHOL INDUCED.
P:
IVF 2 units-2unitsNS, 1Unit RL@75ml/hr
Inj. DOXY 100mg iv/BD
Inj. THAIMINE 200mg in 100ml NS iv/BD
SYP. LACTULOSE 15ml HS






Comments
Post a Comment