FINAL PRACTICAL:LONG CASE
This is an E log book to discuss our patient's de-identified health data shared after taking his guardian's signed informed consent. Here we discuss our individual patient problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable comments in comment box are most welcomed
I have been given this case to solve in an attempt to understand the topic of "Patient clinical data analysis" to develop my competency i reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
K.TEJARSHINI
Hall Ticket No:1701006083
June,06,2022.
MEDICINE CASE DISCUSSION:
A 40year old male,painter by occupation,resident of Bhongir came to the hospital with complaints of,
*Shortness of breath since 1week
*Chest pain on left side since 5days
HISTORY OF PRESENTING ILLNESS:
-Patient was apparently asymptomatic 1month back then he developed shortness of breath
Grade 1 which was Insidious in onset,gradually progressive which get aggravated while walking and get relieved by taking rest.
-Suddenly there is aggravation of symptoms short ness of breath which progressed from grade 1-2, aggravated on postural variation (lying on left side) and get relieved on sitting position.
-Associated with Chestpain which is pricking type non radiating type of pain.
There is history of choking while eating so he didn't eat solid foods he eats only liquid food.
-loss of weight (about 10kgs in past 1year)
-Decreased appetite.
-He stopped working as painter since 1year because of increased weakness,fatigue.
-No History of cough,evening rise of temperature,fever, haemoptysis,orthopnea,PND, palpitations.
PAST HISTORY:
No history of similar complaints in past
Known case of Diabetes and on medication past 3years(Metformin 500mg,Glimiperide1mg tablet)
Not a Known case of TB,HTN, CAD,ASTHMA, EPILEPSY,
PERSONAL HISTORY:
Appetite:Normal (Decreased since 1year)
Diet:Mixed
Bowel and bladder habits :regular
Sleep:Adequate(but disturbed from past few days)
Addictions:
Alcohol started when he was 15to20 years of age (90ml per day) but stopped 1month back.
Smoking was started when he was 15 to 20years of age (10 cigarettes per day) but stopped 1year back.
FAMILY HISTORY:
No similar complaints in the past
GENERAL EXAMINATION:
Patient is examined in a well lit room with adequate exposure, after taking the consent of the patient.
He is conscious, coherent and cooperative, moderately built and nourished.
No signs of pallor, edema, icterus, cyanosis, clubbing, Generalized lymphadenopathy.
VITALS:
Temperature : Afebrile
Pulse rate : 139beats/min
BP : 110/70 mm Hg
RR : 45 cpm
SpO2 : 91% at room air
GRBS : 201mg/dl
Clinical Pictures:
RESPIRATORY SYSTEM EXAMINATION:
INSPECTION:
Shape of chest is elliptical,
B/L asymmetrical chest,
Trachea appears in central position,
Expansion of chest- Right- normal, left-decreased,
Movements of chest decreased on left side,
Use of Accessory muscles is present.
PALPATION:
No local rise of temperature,non tender
trachea is deviated to the right,
Measurement:
AP: 24cm
Transverse:28cm
Right hemithorax:42cm
left hemithorax:40cm
Circumferential:82cm
Tactile vocal fremitus: decreased on left side- Inter scapular area(ISA),
Infra scapular area(ISA),
Axillary area(AA),
Infra axillary areas(Infra AA).
PERCUSSION: Stony dull note present in left side ISA, InfraSA, AA, IAA.
- AUSCULTATION:
B/L air entry present, vesicular breath sounds heard,
Decreased intensity of breath sounds in left SSA,IAA,
Absent breath sounds in left ISA.
- CVS EXAMINATION:
S1,S2 heard
No murmurs. No palpable heart sounds.
JVP: normal
Apex beat: heard in left 5th intercostal space 1.5cm medial to midclavicularline.
- PER ABDOMEN:
Soft, Non-tender
No organomegaly
Bowel sounds heard
no guarding/rigidity
- CNS EXAMINATION:
No focal neurological deficits
Gait- NORMAL - Sensory and motor system examination:normal
- Cerebellar functions :normal
- Reflexes: intact
PROVISIONAL DIAGNOSIS:
Left side PLEURAL EFFUSION
with DM since 3years.
INVESTIGATIONS:
FBS: 213mg/dl
HbA1C: 7.0%
Hb: 13.3gm/dl
TC: 5,600cells/cumm
PLT: 3.57
Serum electrolytes:
Na: 135mEq/l
K: 4.4mEq/l
Cl: 97mEq/l
Serum creatinine: 0.8mg/dl
LFT:
TB: 2.44mg/dl
DB: 0.74mg/dl
AST: 24IU/L
ALT: 09IU/L
ALP: 167IU/L
TP: 7.5gm/dl
ALB: 3.29gm/dl
LDH: 318IU/L
Blood urea: 21mg/dl
Needle thoracocentesis
-under strict aseptic conditions USG guidance 5%xylocaine instilled 20cc syringe 7th intercoastal space in mid scapular line left hemithorax pale yellow coloured fluid of 400ml of fluid is aspirated diagnostic approach.
PLEURAL FLUID:
Protein: 5.3gm/dl
Glucose: 96mg/dl
LDH: 740IU/L
TC: 2200
DC: 90% lymphocytes
10% neutrophils
ACCORDING TO LIGHTS CRITERIA: (To know if the fluid is transudative or exudative.
Serum Protein ratio: >0.5
Serum LDH ratio: >0.6
LDH>2/3 upper limit of normal serum LDH
Proteins >30gm/L
My Patient:
Serum protein ratio:0.7
Serum LDH: 2.3
INTERPRETATION: As 2 values are greater than the normal we consider as an EXUDATIVE EFFUSION.
(confirmation after pleural fluid C/S analysis)
CHEST X RAY :
On day of admission
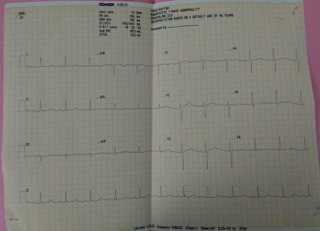
ECG:
TREATMENT:
Medication:
- O2 inhalation with nasal prongs with 2-4 lt/min to maintain SPO2 >94%
- Inj. Augmentin 1.2gm/iv/TID
- Inj. Pan 40mg/iv/OD
- Tab. Pcm 650mg/iv/OD
- Syp. Ascoril-2tsp/TID
- DM medication taken regularly
Advice:
- High Protein diet
- 2 egg whites/day
- Monitor vitals
- GRBS every 6th hourly
No


.jpeg)







Comments
Post a Comment