Medicine Case Discussion
29 YEARS OLD FEMALE WITH C/O BILATERAL JOINT PAINS INVOLVING BOTH UPPER AND LOWER LIMBS , GENERALIZED WEAKNESS and ITCHY SKIN LESIONS SINCE 10 MONTHS.
Cheif complaints of:
* Bilateral joint pains in upper and lower limbs(knees, hip, ankle, shoulder, elbow, wrist, including small joints of foot ) since 10 months.
She is also complaining of pain in both arms since 10months
Generalised weakness since 10 months
* Inability to comb the hair, difficulty in walking and inability to sit down.
•Itchy lesions over the face,upper aspect of the chest, neck and back of the neck and upper trunk with dark coloured lesions over the knuckles since 10 months.
History Of present illness:-
•Patient was apparently asymptomatic 10 months ago,after which she complained of bilateral symmetrical multiple joint pains involving all joints and it's severe in the knees which was insidious in onset, gradually progressive,pricking type of pain continuous type but more during evening times aggravated on walking and relieved on medication .
Order of involvement of joints :
Bilateral knee joints-hip joints and ankle joints and joints of foot -shoulder joints-elbow joints-wrist joints.
Associated with morning stiffness that she cannot get out of bed.
•Around the same time she developed itching over neck and upper chest area.The area was initially red and turned black due to itching.
•H/o Dark coloured skin lesions over the knuckles since 10 months
•H/o photosensitivity present (Itching increases on sun exposure)
•H/o Alopecia since 10 months. It was gradually progressive leading to severe hair loss over the past 10 months. Associated with thinning of hair.
•H/o bilateral pitting type of pedal Edema upto ankle and Edema over the dorsal aspect of hands.
•H/o generalised weakness since 10 months.
•H/o Dfficulty in walking and difficulty to sit down and also difficulty in getting up from sitting position.
H/o distal muscle weakness manifested in the form of : difficulty in mixing food, eating with hands, dressing and undressing, combing of hair.
•H/o proximal muscle weakness manifested in the form of : difficulty in getting up from squatting position, getting objects present at a height.
•H/o weight loss of 4-5 kgs over the last 10 months.
•H/o Oral ulcers on and off since 10 months,and she is unable to eat spicy foods.
•H/o vaginal discharge since 7-8 months. It was initially curdy white discharge which later changed to watery discharge. Associated with itching.
•H/o Genital ulcers on and off since 7 months.
•Dyspnea on exertion (NYHA- 3),gradually progressive since 4-5 months
*Fever on and off episodes fever is present when she is having severe pain .
She went to hospital in LB Nagar,Nampally hospitals it cannot controlled.
After coming to the hospital she is complaining of cough since saturday for which she is put on Dextromethorphan syrup.
No history of back pain
No history of cold exacerbation of symptoms
No history of bowel and bladder involvement
Past History:-
No similar complaints in the past.
•Not a k/c/o DM, HTN,TB, epilepsy, Asthma, CVA, CAD.
Menstrual History:-
•Age of menarche:-11 years
•Duration of cycle :- 3/28 days
•Regular cycle with no pains and no clots.
Marital History:-
•Age at marriage:19years
•Non consanguinous marriage
•Primary infertility (Nulligravida)
Personal History:-
•Diet- Mixed
•Appetite- Decreased
•Sleep- Inadequate since 10 months
•Bowel and bladder habits- Regular
•No addictions
No known drug allergies
Family History
•Not significant
General Examination:-
•Patient is conscious, coherent and cooperative.Well Oriented to time, place and person.
•She is moderately built and moderately nourished.
•Pallor- Present
Icterus-Absent
•cyanosis-Absent
•clubbing-Absent
•lymphadenopathy-Absent
•Pedal Edema- Present
On Examination:-
- Diffuse mottled erythematous hyperpigmentation (Heliotrope rash) noted on B/L cheeks, nose(bridge) involving nasolabial folds, ears, neck extending onto upper chest and back forming a ‘V’ on anterior chest (Shawl sign) and (V sign).
*Pigmentation of B/L extensor surfaces of PIP, DIP joints noted (Gottron's papules).
* Mottled erythematous lesions on the palms.
Vitals:-
•Temperature- Afebrile
•BP- 130/80 mm Hg
•PR- 102 bpm
•RR- 14 cpm
•SpO2- 99% @ RA
EXAMINATION OF JOINTS:
Joints. tenderness. Restriction of movement
DIP. + _
PIP. + -
Wrist. + _
Elbow. + -
Shoulder. + +
Atlanto axial joint. + _
Hip joint. + _
Knee joint. + +
Ankle joint. + +
Inter phalangeal joints of toes. +. +
Systemic Examination:-
•HEMOGRAM:-
Normocytic Normochromic blood picture with MILD LEUCOPENIA.
•COMPLETE URINE EXAMINATION:-
Serum Creatinine:

Serum Electrolytes:
BLOOD SUGAR-RANDOM:-
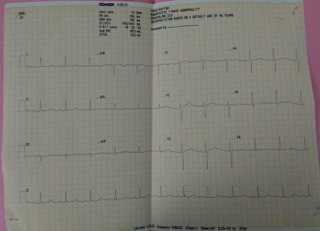
ECG:
Cortical calcifications noted at upper pole of Rt.Kidney
*Raised Echogenicity of B/L Kidneys.
•SEROLOGY - Negative
•RA Factor- Negative
•CRP- Negative
*Provisional Diagnosis:-
Dermatomyositis with vaginal candidiasis
SLE under evaluation
*Referrals:-
•Dermatology referral was taken.
Treatment:-
•On 08/01/2022:-
1.Tab.Fluconazole 150mg/PO/stat
2.Candid cream L/A
3.Tab pan 40 mg PO/OD
4.Tab Ultracet 1/2 tab/PO/Q.I.D
5.Syrup.Grilinctus BM 10ml/PO/T.I.D
6.Syrup.Mucaine Gel 10ml/PO/T.I.D
•On 09/01/2022:-
1.Tab.Fluconazole 150mg/PO/stat
2.Candid cream L/A
3.Tab pan 40 mg PO/OD
4.Tab Ultracet 1/2 tab/PO/Q.I.D
5.Syrup.Grilinctus BM 10ml/PO/T.I.D
6.Syrup.Mucaine Gel 10ml/PO/T.I.D
On 10/01/2022:-
1.Tab.Fluconazole 150mg/PO/stat
2.Candid cream L/A
3.Tab pan 40 mg PO/OD
4.Tab Ultracet 1/2 tab/PO/Q.I.D
5.Syrup.Grilinctus BM 10ml/PO/T.I.D
6.Syrup.Mucaine Gel 10ml/PO/T.I.D
On 11/01/2022:-
1.Tab.Fluconazole 150mg/PO/stat
2.Candid cream L/A
3.Tab pan 40 mg PO/OD
4.Tab Ultracet 1/2 tab/PO/Q.I.D
5.Syrup.Grilinctus BM 10ml/PO/T.I.D
6.Syrup.Mucaine Gel 10ml/PO/T.I.D


















Comments
Post a Comment