GENERAL MEDICINE CASE DISCUSSION
General medicine case discussion
19/10/2021
This is is an online E log book to discuss our patient's deidentified health data shared after taking his/her/guardian's signed in formed consent.Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems withcollective current best evidence-based inputs.This e-log book also reflects my patient centered online learning protfolio and your valuable inputs on comment box is welcome.
E LOG MEDICINE CASE
Roll no : 61
2017 Batch
I''ve been given this case to solve in an attempt to understand the topic of "PATIENT CLINICAL DATA ANALYSIS" to develop my competency in reading and comprehending clinical data including history,clinical findings,investigations and come up with Diagnosis and treatment plan.
CHEIF COMPLAINTS:
A 35 Year old woman presented to the opd complained of fever ,cough since 1 week . vomiting since 2 days from the date of admission.
History of presenting illness:
Admitted on 17/10/2021.
Patient was alright 1 week back then she presented with fever which is low grade , intermittent,no diurnal variations,relieved on medication.
Fever not associated with chills and rigor.
She also complained of cough which is non-productive.
Since 2 days she also complained of vomiting 1 episode/day, which is non-projectile,non bilious ,not blood stained vomiting.
Associated with nausea.
Past history;
There is a history of attack of poliomyelitis when she was at the age of 6 years,Studied till 1 st grade, then she developed sudden onset of left upper limb and lower limb weakness (Hemiparesis) she was taken to hospital near nalgonda (marrigudem) there they prescribed on oral medication for 2 yrs , over time she regained some power in Lt UL and LL . She does her own household chores and takes care of herself and others.she also taken to the another hospital there is no improvement.
There is no history of HTN,DM, EPILEPSY.
Family history:
Insignificant
Personal History:
Appetite: normal
There is decreased appetite since 1 week
Diet:Mixed
Bowel and bladder habits:regular
Sleep: adequate
Since 1 week there is inadequate sleep.
General examination:
Conscious, coherent, co-operative
Moderately built,nourished
Vitals :
Temp - 98.1 F
PR - 95/min
RR - 20/min
BP - 100/80mmhg
SpO2 - 99% at room air
GRBS - 138 mg%
SYSTEMIC EXAMINATION:
RESPIRATORY SYSTEM:
CVS:
S1,S2 +
P/A:
Soft ,Non tender
Bowel sounds +
CNS -
Tone increased in left upper limb and lower limb
Power :
Right Left
UL 5 4
LL 5 4
Reflexes :
Right Left
B 2+ -
T 2+ -
S 2+ -
K 3+ 3+
A + +
P Flexion bilaterally
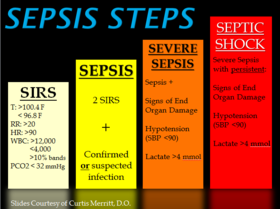
Provisional Diagnosis :
-Dengue fever with thrombocytopenia ( NS1 positive ) -35,000 outside
Yesterday- 61,000
INVESTIGATIONS:
17/10/2021,
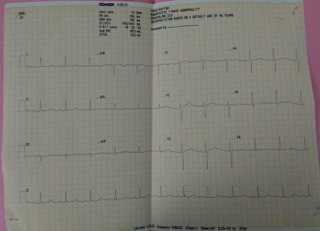
CHEST X-RAY:
HEMOGRAM,RFT,LFT,SEROLOGY:
TPR CHART:
IVF NS 100ml IV/hr ,IVF RL 100ml IV/hr
Inj.pantop 40mg IV OD
Inj. Zofer 4mg IV TID
19/10/2021:
Plenty of oral fluids
IVF 20 NS @125ml/hour, 10 RL continous infusion
Inj.PANTOP 40mg/iv/OD
Inj.ZOFER 4mg/iv/OD
Syrup AMBROXOL 10ml/po/TID with one glass of water
Tab.DOLO 650mg/po/TID
TEMP CHARTING 4th Hourly
W/F BLEEDING MANIFESTATIONS
PLATELET,PCV 12th HOURLY
Monitor VITALS
I/O CHARTING.
20/10/2021:
IVF NS 75ml iv /hr
IVF RL 75ml iv /hr
IVF DNS 75ml iv /hr
Inj PANTOP 40mg /iv/OD
Inj.ZOFER 4mg/iv/OD
Tab.DOLO 650mg/po
Inj.NEOMOL 100ml iv/SOS
Syp.GRILINCTUS 10ml po/SOS
Syrup.AMBROXOL TID.









Comments
Post a Comment