E LOG MEDICINE CASES
CASE OF A 60 YEAR OLD MALE WITH CHRONIC RENAL FAILURE WITH METABOLIC ACIDOSIS WITH K/C/O OF HYPERTENSION.
June 7th 2021.
This is an online E log book to discuss our patient's deidentified health data shared after taking his/her/guardian's signed in formed consent.Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence-based inputs.This e-log book also reflects my patient centered online learning protfolio and your valuable inputs on comment box is welcome.
K.Tejarshini,
Roll no:61, 8th SEM,
7/06/21.
I''ve been given this case to solve in an attempt to understand the topic of "PATIENT CLINICAL DATA ANALYSIS" to develop my competency in reading and comprehending clinical data including history,clinical findings,investigations and comeup with Diagnosis and Treatment plan.
Following is the view of my case:(under the guidance of Dr.Divya ma'am).
CASE DISCUSSION:
Date of admission:7/06/21
A 60 YEAR OLD MALE the CAME TO HOSPITAL ON 7/06/21 WITH,
CHEIF COMPLAINTS :
SHORTNESS OF BREATH since 4 days present even at rest.
Pedal edema since 4 days.
Decreased urine output since 4 days.
HISTORY OF PRESENTING ILLNESS :
Patient was apparently asymtomatic 3 years back,then he had a history of Shortness of breath,pedal edema,decreased urine output ,facial puffiness,fever,chest heaviness,knee pains for 5 days for which he admitted to the hospital on 2/01/19.
Now the symptoms got exacerbated since 4 days with history of SOB which is present even on rest( grade -4), pedal edema which is bilateral pitting type upto the knees and also decreased urine output since 4days.
There is no history of palpitations,cough,fatigue.
His HB is 11.5,
Albumin levels in urine is trace,
B.P:190/110mm of Hg.
On 2/01/19:
Serum creatinine:3.2 ,k+ :3.3
3/01/19:
Serum creatinine:3.8 ,k+:2.7
4/01/19:
Serum creatinine:4 ,k+:4.3
6/01/19:
Serum creatinine:3.8
9/1/19:
Serum creatinine:3.2 , Blood urea:95
Albumin:3+
2/08/19:
Serum creatinine:4.3 , Albumin:2+ ,pus cells:8-10
4/08/2020:
Serum creatinine:5.2
20/01/2020:
Serum creatinine:4.1 ,HB:8 , Albumin:trace.
31/01/2020:
EF:50 % concentric LVH ,mild LV systolic dysfunction (+) ,HB:7.5
26/12/2020:
Serum creatinine:5.0 ,uric acid:8.5 , Albumin :(+) ,pus cells:6-8
4/01/2021:
Nephro opinion taken I/V/O -renal failure.
31/5/2021:
Serum creatinine:8.2 ,HB:6.5 ,K+:3.5.
1/06/2021:
EF:55% ,MAC (+).
PAST HISTORY :
He has similar complaints in the past.
Mild dilated LA/LV
Concentric LVH
Min.Pericardial effusion.
He is a Known case of hypertensive since 3years and he is on treatment.
There is also a history of asthma,and he is on treatment.
There is no history of DB,CAD,TB.
No history of previous surgeries.
PERSONAL HISTORY :
Appetite: Normal
Diet:Mixed
Sleep:adequate
Bowels: irregular
Micturition: Decreased micturition since 1year.
There is no history of food and drug allergies.
Habits:
There is a history of regular alcohol consumption since 30yrs(chronic alcoholic).
He is also a chronic smoker since 30yrs and stopped smoking 2yrs back .
FAMILY HISTORY :
Insignificant family history.
GENERAL EXAMINATION :
Patient is conscious, coherent and co-operative.
Oriented to time,place, person.
Moderately built,nourished.
Pallor:absent,
Icterus:absent,
Cyanosis: absent,
Clubbing of fingers/toes: absent,
Oedema of legs:(+) bilateral pitting type upto the knee
VITALS:
Temperature: afebrile,
Pulse:82beats/min,
Blood pressure:110/70mm of Hg,
Respiratory rate:17cycles/min,
Spo2: 100% at room air.
SYSTEMIC EXAMINATION :
CVS:
S1,S2 Sounds heard,
No audible murmurs.
RESPIRATORY SYSTEM :
Bilateral air entry present(BAE),
Dyspnea is present,
Diffuse wheeze is present,
Normal vesicular breath sounds are heard,
No adventitious sounds heard.
ABDOMEN:
Shape: Scaphoid,
Soft and non tender abdomen,
No organomegaly,
Bowel sounds:heard.
CNS:
Intact,
Higher mental functions intact,
Reflexes present.
PROVISIONAL DIAGNOSIS :
CHRONIC RENAL FAILURE WITH METABOLIC ACIDOSIS WITH K/C/O OF HYPERTENSION.
INVESTIGATIONS ORDERED :
HEMOGRAM,CUE,RFT,LFT,ABG,ECG,CHEST X RAY.
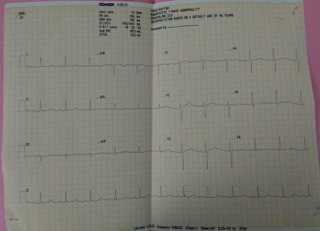
ECG :

7/06/2021;8am
ABG :
pH: 7.150
Pco2: 15.1mmHg
Po2: 126mmHg
Spo2: 98.1mmHg
Hco3: 5.1meq/l
St(Hco3): 7.6meq/l
CBP :
HB:5.6gm/dl
Total count:10,500 cells/mm3
Neutrophils:94%
Lymphocytes:3%
Eosinophils:1%
Monocytes:2%
Basophils:0%
RFT :
serum creatinine:12.8mg/dl
Urea:224mg/dl
Uric acid:11.6mg/dl
Ca+2:7.0mg/dl
Na+:137meq/l
K+:4.9meq/l
Cl-:98meq/l
LFT :
Total Bilirubin:0.96mg/dl
Direct Bilirubin:0.20mg/dl
SGOT(AST):26IU/L
SGPT(ALT):10IU/L
Alkaline phosphate:338IU/L
Total proteins:5.6gm/dl
Albumin:3.3gm/dl
A/G ratio:1.54
CHEST X-RAY :
USG REPORT :
TREATMENT :
7/06/2021;2:30am
1)Inj.LASIX 40mg IV/BD
(If SBP >= to 110mmof Hg)
2)TAB.MET-XL 12.5mg PO/OD
3)TAB.ARKAMINE 0.1mg PO/TID
4)TAB.NODOSIS 500mg PO/TID
5)TAB.DROFER XT PO/BD
6)TAB.PCM 500mg PO/SOS
7)TAB.PANTOP 40mgPO/OD
8)NEB.With BUDECORT,DUOLIN-8TH HOURLY
9)BP/PR/TEMPERATURE/R.R-Monitor 4th hourly
10)I/O-Charting.
7/06/2021;8:00am:
Complaint of SOB decreased compared to yesterday.
O/E:
Patient-Conscious,Coherent, Co-operative
Afebrile;96.6F
PR:88bpm, regular
BP:130/70mmofHg
R.R:20cpm
CVS:S1 S2 heard
CNS: Oriented to T/P/P
R/S:BAE(+), Clear
P/A:Soft
TREATMENT:
1)SALT RESTRICTION:<2.4gm/day
2) FLUID RESTRICTION:<1.5L/day
3)Inj.LASIX 40mg IV/BD(If SBP>=110mmofHg)
4)TAB.NODOSIS 500mg PO/TID
5)TAB.PANTOP 40mg PO/OD
6)TAB.DROFER XT PO/BD
7)NEB.With BUDECORT, DUOLIN-8TH HOURLY
8)TAB.ARKAMINE 0.1mg PO/OD
9)BP/P.R/TEMPERATURE/R.R-Monitor 4th hourly
10)I/O -Charting
I would like to thank Dr.Rakesh Biwas sir for giving me this opportunity and also thank's to Dr.Divya ma'am for guidance.








Comments
Post a Comment