Medicine case discussion
Online blended bimonthly assignment towards summative assessment for the month of May 2021
Name:K.Tejarshini
Roll number:61
Date:may 31 2021
I have been given the following cases to solve in an attempt to understand the topic of 'patient clinical data analysis' to develop my competency in reading and comprehending clinical data including history , clinical findings ,investigations and diagnosis to come up with a treatment plan
http://medicinedepartment.blogspot.com/2021/05/online-blended-bimonthly-assignment.html
Below are my answers to the medicine assignment based on my comprehension of my cases
1) PULMONOLOGY:
CASE 1
A 55 year old female patient, a resident of Miryalaguda and farmer by occupation came to the hospital on 17/5/21 with the chief complaints ofshortness of breath, pedal edema andfacial puffiness.
https://soumyanadella128eloggm.blogspot.com/2021/05/a-55-year-old-female-with-shortness-of.html
1Q) what is the evolution of the symptomatology in this patient interms of an event timeline and where is the anatomical localisation for the problem and what is the primary etiology of the patient problem ?
1Ans)Evolution of symptomatology
1st episode of sob - 20 yr back
2nd episode of sob - 12 yr back
From then she has been having yearly episodes for the past 12 yrs
Diagnosed with diabetis - 8yrs back
Anemia and took iron injections - 5yr ago
Generalised weakness - 1 month back
Diagnosed with hypertension - 20 days back
Pedal edema - 15 days back
Facial puffiness- 15 yrs back
Anatomical location of problem - lungs
Primary etiology of patient- usage of chulha since 20 yrs might be due to chronic usage
2Q)what r the mechanism of action indication and efficacy over placebo of each of the phramacological and nonphramacological interventions used for this patient?
2Ans)~Head end elevation :# MOA;
.improves oxygenation
.decreases incidence of VAP
.increases hemodynamic performance
.increases end expiratory lung volume
.decreases incidence of aspiration
#Indication: .head injury
.meningitis
.pneumonia
~ oxygen inhalation to maintain spo2
~Bipap:non invasive method
#MOA :assist ventilation by delivering positive expiratory and inspiratory pressure with out need for Endotracheal tube intubation
3. Cause for current acute excerbation -
It could be due to:
1)Any infection s of airways or lungs
Bacterial:H.influenzae,s.pneumoniae,M.catarrhalisetc
Viral:Covid, enterovirus,picornavirus, rhinovirus etc.
2)Allergens
eg:pollen,wood, cigarette smoke, pollution
In this patient may be it can result due to usage of chulha for past 20 years.
3)Toxins including a variety of different chemicals.
4)Airpollution.
5)Failing to follow a drug therapy
eg:improper use of an inhaler.
4.could the ATT affected her symptoms if so how?
Yes ATT can effect her symptoms.
Isoniazid toxicity causes profound metabolic acidosis: respiratory centre in the brainstem is stimulated and hyperventilation develops in an effort to compensate for the acidosis
Rifampicin-Drug induced flu-like syndrome, possibly related to production of rifampicin-dependent antibody symptoms associated with it are fever with chills and rigor,dry cough,mild breathlessness, rhinorrhea.
Isoniazid and rifampcin -nephrotoxic - raised RFT was seen.
5)What could be the causes for her electrolyte imbalance?
-Due to COPD,there is hypercapnic acidosis, hypoxemia.The systemic response to hypercapnia has the effect of reducing the renal blood flow due to noradrenaline release via chemoreceptor stimulation and peripheral vasodilation,leading to renal vasoconstriction and as a result,increasing water and sodium retention with the final effect of edema and hyponatremia chloride ion follows sodium ion.
-In heart failure with low cardiac output state, activation of the RAAS system serves as a compensatory mechanism to maintain Cardiac output and also reduced renal blood flow and sodium delivery to the distal tubule leads to renin release,which is further exacerbated by increased sympathetic tone in which elevated levels of vasopressin causes increase in water reabsorption and retention which will disproportionately expand the plasma volume ,thus resulting in dilutional hyponatremia.
2) NEUROLOGY:
A)
Link to patient details
https://143vibhahegde.blogspot.com/2021/05/wernickes-encephalopathy.html
A 40year old male presented with chief complaints of irrelevant talking and decreased food intake since 9days.
He was conscious but oriented to time, person and place only from time to time.
He also had short term memory loss since 9days, where he couldn't recognize family members from time to time
Previously, he had 2-3episodes of seizures, one being one year ago and the most recent being 4months ago. The most recent one, he had developed seizures following cessation of alcohol for 24hours.
Questions:
1) what is the evolution of the symptomology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Ans: The patient is a chronic alcoholic, he drinks about 3-4quarters/day.he had developed seizures following the cessation of alcohol for 24hours it is due to the following reason:-alcohol affects the way in which nerve cells communicate. receptors are specialized proteins on the surface of nerve cells that receive chemical signals from one another. With long-term alcohol consumption, receptors affected by alcohol undergo adaptive changes in an attempt to maintain normal function.
Two important brain communication systems affected by alcohol involve the neurotransmitters:gamma-aminobutyric acid and glutamate.
The GABA system:
GABA is an inhibitory neurotransmitter that helps to regulate brain function by rendering nerve cells less sensitive to further signaling. single doses of alcohol facilitate the inhibitory function of the GABA receptor, contributing to alcohol intoxicating effects. During withdrawal, brain GABA levels fall below normal and GABA activity declines. The combination of reduced brain GABA levels and GABAa receptor sensitivity may be contributed an adaptation to the presence of alcohol. In the absence of alcohol, the resulting decrease in inhibitory function may contribute to Symptoms of nervous system hyperactivity associated with both acute and protracted AW.
The glutamate system:
The major excitatory neurotransmitter in the brain is glutamate, which communicates with three major subtypes of glutamate receptors. Among these, the N-methyl-D-aspartate (NMDA) receptor plays a role in memory, learning, and the generation of seizures. Alcohol inhibits the excitatory function of the NMDA receptor in laboratory studies at concentrations associated with mild to moderate alcohol intoxication in humans. As with the increased inhibitory function of the GABAA receptor, the decreased excitatory function of the NMDA receptor is consistent with alcohol’s general sedative effect. Long-term alcohol administration produces an adaptive increase in the function of NMDA receptors. Acute AW activates glutamate systems. In turn, AW seizures are associated with increased NMDA receptor function. Persistent alterations in NMDA receptor function may potentiate the neurotoxic and seizure-inducing effects of increased glutamate release during withdrawal.
The symptom: irrelevant talking, decreased food intake, tremors, sleep disturbance is due to the following reason: chronic alcohol consumption causes thiamine deficiency due to impaired absorption of thiamine from the intestine, a possible genetic predisposition, inadequate diet, reduced storage of thiamine in the liver and other nutritional deficiencies.
THE PATHOPHYSIOLOGY:
Thiamine, one of the first B vitamins to be discovered also known as Vitamin B1, is a coenzyme that is essential for intricate organic pathways and plays a central role in cerebral metabolism. This vitamin acts as a cofactor for several enzymes in the Krebs cycle and the pentose phosphate pathway, including alpha-keto-glutamic acid oxidation and pyruvate decarboxylation. Thiamine-dependent enzymes function as a connection between glycolytic and citric acid cycles. Therefore, deficiency of thiamine will lead to decreased levels of alpha-keto-glutarate, acetate, citrate, acetylcholine and accumulation of lactate and pyruvate. This deficiency can cause metabolic imbalances leading to neurologic complications including neuronal cell death. Neuronal death in the mammillary bodies and thalamus were implicated in multiple cases of Wernicke encephalopathy studied. Studies involving computed tomography (CT) and magnetic resonance imaging (MRI) of patients with Wernicke encephalopathy revealed lesions in the thalamus with dilated ventricles and volume loss in the mammillary bodies. The lesions are usually symmetrical in the midbrain, hypothalamus, and cerebellum.
The kidneys have an important job as a filter for harmful substances .alcohol causes changes in the function of the kidneys and makes them less able to filter the blood .alcohol also affects the ability to regulate fluid and electrolytes in the body. In addition, alcohol can disrupt hormones that disrupt hormones that affect kidney function .people who drink too much are more likely to have high blood pressure. High blood pressure is a common cause of kidney disease. The increase in levels of urea, creatinine, uric acid leads to uraemic encephalopathy. which causes asterixis.
the deficiency of thiamine and increase in levels of toxins in the body due to renal disease is the primary etiology of the patient's problem.
2)what are the mechanism of action, indication, and efficacy over placebo of each of the pharmacological and nonpharmacological interventions used for this patient?
Ans: I) Thiamine helps the body cells change carbohydrates into energy. It has been used
as a supplement to cope with thiamine deficiency
ii)Lorazepam binds to benzodiazepine receptors on the postsynaptic GABA-A ligand-gated chloride channel neuron at several sites within the central nervous system.it enhances the inhibitory effects of GABA, which increases the conductance of chloride ions into the cell
iii)pregabalin subtly reduces the synaptic release of several neurotransmitters, apparently by binding to alpha2-delta subunits, and possibly accounting for its actions invivo to reduce neuronal excitability and seizures.
iv)Lactulose is used in preventing and treating clinical portal-systemic encephalopathy .its chief mechanism of action is by decreasing the intestinal production and absorption of ammonia.
v)Potchlor liquid is used to treat low levels of potassium in the body.
3)why have neurological symptoms appeared this time, that were absent during withdrawal earlier ? what could be a possible cause for this time?
Due to excess thiamine deficiency and excess toxins accumulation due to renal disease caused by excess alcohol addiction.
4)what is the reason for giving thiamine in this patient?
chronic alcohol consumption causes thiamine deficiency due to impaired absorption of thiamine from the intestine,Thiamine, one of the first B vitamins to be discovered also known as Vitamin B1, is a coenzyme that is essential for intricate organic pathways and plays a central role in cerebral metabolism. This vitamin acts as a cofactor for several enzymes in the Krebs cycle and the pentose phosphate pathway, including alpha-keto-glutamic acid oxidation and pyruvate decarboxylation. Thiamine-dependent enzymes function as a connection between glycolytic and citric acid cycles. Therefore, deficiency of thiamine will lead to decreased levels of alpha-keto-glutarate, acetate, citrate, acetylcholine, and accumulation of lactate and pyruvate. This deficiency can cause metabolic imbalances leading to neurologic complications including neuronal cell death.
5)what is the probable cause for kidney injury in this patient?
The kidneys have an important job as a filter for harmful substances .alcohol causes changes in the function of the kidneys and makes them less able to filter the blood .alcohol also affects the ability to regulate fluid and electrolytes in the body. In addition, alcohol can disrupt hormones that disrupt hormones that affect kidney function .people who drink too much are more likely to have high blood pressure. High blood pressure is a common cause of kidney disease.
6)what is the probable cause for the normocytic anaemia?
alcohol causes iron deficiency or iron overload due its affect on production of new blood cells organs i.e,bonemarrow and the metabolism of iron .alocohol causes a affect on progenitor cells of blood causing decreased WBC .RBC.alochol decreases iron absorption from intestine .
7)could chronic alcohlism have aggravated the foot ulcer formation ?if yes and why ?
yes,As the patient is diabetic the chance of ulcer formation increases .in a patient of chronic alcoholic theimmune system is weak due to the affect on blood cells formation and iron absorption.due to this healing of an ulcer dampens.
B)Link to patient details:
https://kausalyavarma.blogspot.com/2021/05/a-52-year-old-male-with-cerebellar.html?m=1
A 52 year old male came to the hospital 2days back presenting with slurring of speech and deviation of mouth lasted for one day and resolved on the same day.
Questions:
1) What is the evolution of the symptomology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patients problem?
ANS. Timeline of the patient is as follows-
7 days back- Patient gave a history of giddiness that started around 7 in the morning; subsided upon taking rest; associated with one episode of vomiting
4 days back- Patient consumed alcohol; He developed giddiness that was sudden onset, continuous and gradually progressive. It increased on standing and while walking.
H/O postural instability- falls while walking
Associated with bilateral hearing loss, aural fullness, presence of tinnitus
Associated vomiting- 2-3 episodes per day, non projectile, non bilious without food particles
Present day of admission- Slurring of speech, deviation of mouth that got resolved the same day
Anatomical location- There is a presence of an infarct in the inferior cerebellar hemisphere of the brain.
Etiology- Ataxia is the lack of muscle control or co-ordination of voluntary movements, such as walking or picking up objects. This is usually a result of damage to the cerebellum (part of the brain that controls muscle co-ordination)
Many conditions cause cerebellar ataxia- Head trauma, Alcohol abuse, certain medications eg. Barbituates, stroke, tumours, cerebral palsy, brain degeneration etc.
In this case, the patient has hypertension for which he has been prescribed medication that he has not taken. Stroke due to an infarct can be caused by blockade or bleeding in the brain due to which blood supply to the brain is decreased, depriving it of essential oxygen and nutrients. This process could’ve caused the infarct formation in the cerebellar region of the brain, thus causing cerebellar ataxia.
2) What are the mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
ANS.
A) Tab Vertin 8mg- This is betahistine, which is an anti- vertigo medication
MOA- It is a weak agonist on H1 receptors located on blood vessels of the inner ear. This leads to local vasodilation and increased vessel permeability. This can reverse the underlying problem.
Indications- Prescribed for balance disorders. In this case it is used due to patients history of giddiness and balance issues.
B) Tab Zofer 4mg- This is ondanseteron- It is an anti emetic
MOA- It is a 5H3 receptor antagonist on vagal afferents in the gut and they block receptors even in the CTZ and solitary tract nucleus.
Indications- Used to control the episodes of vomiting and nausea in this patient.
C) Tab Ecosprin 75mg- This is aspirin. It is an NSAID
MOA- They inhibit COX-1 and COX-2 thus decreasing the prostaglandin level and thromboxane synthesis
Indications- They are anti platelet medications and in this case used to prevent formation of blood clots in blood vessels and prevent stroke.
D) Tab Atorvostatin 40mg- This is a statin
MOA- It is an HMG CoA reductase inhibitor and thus inhibits the rate limiting step in cholesterol biosynthesis. It decreases blood LDL and VLDL, decreases cholesterol synthesis, thus increasing LDL receptors in liver and increasing LDL uptake and degeneration. Hence plasma LDL level decreases.
Indications- Used to treat primary hyperlipidemias. In this case it is used for primary prevention of stroke.
E) Clopidogrel 75mg- It is an antiplatelet medication
MOA- It inhibits ADP mediated platelet aggregation by blocking P2Y12 receptor on the platelets.
Indications- In this case it decreases the risk of heart disease and stroke by preventing clotting
F) Thiamine- It is vitamin B1
It is naturally found in many foods in the human diet. In this case, the patient consumes excess alcohol- so he may get thiamine deficiency due to poor nutrition and lack of essential vitamins due to impaired ability of the body to absorb these vitamins.
Indications- Given to this patient mainly to prevent Wernickes encephalopathy- that can lead to confusion, ataxia and opthalmoplegia.
G) Tab MVT- This is methylcobalamin
Mainly given in this case for vitamin B12 deficiency.
3) Did the patients history of denovo hypertension contribute to his current condition?
ANS. A cerebellar infarct is usually caused by a blood clot obstructing blood flow to the cerebellum. High blood pressure that is seen in hypertension (especially if left untreated) can be a major risk factor for the formation of cerebellar infarcts.
Increased shear stress is caused on the blood vessels. The usual adaptive responses are impaired in this case, thus leading to endothelial dysfunction in this case. High BP can also promote cerebral small vessel disease. All these factors contribute to eventually lead to stroke.
4) Does the patients history of alcoholism make him more susceptible to ischaemic or haemorrhagic stroke?
ANS. Meta analysis of the relation between alcohol consumption and increased risk of stroke has mainly weighed in to the formation of two types- ischaemic and haemorrhagic stroke.
Ischaemic stroke- this is more common. This Is caused by a blood clot blocking the flow of blood and preventing oxygen from reaching the brain
Haemorrhagic stroke- occurs when an aneurysm bursts or when a weakened blood vessel leaks, thus causing cerebral haemorrhage
According to a Cambridge study, heavy drinkers have 1.6 more chance of intracerebral haemorrhage and a 1.8 increased chance of subaracnoid haemorrhage. The adverse effect on BP that is seen due to increased drinking is a major stroke risk factor and increase the risk of heart stroke.
Many studies show that with mild and moderate drinking . the risk of ischaemic stroke decreases due to decreased level of fibrinogen which helps in the formation of blood clots. However, heavy alcohol intake is associated with impaired fibrinolysis, increased platelet activation and increased BP and heart rate.
So In this case, his history of alcoholism, coupled with his hypertension definitely could be a causative factor of his current condition.
C) Link to patient details:
http://bejugamomnivasguptha.blogspot.com/2021/05/a-45-years-old-female-patient-with.html
A 45 year old female patient with palpitations,pedal edema,chest pain ,Chest heaviness , radiating pain along left upper limb.
Questions:
1Q)What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
A) *Evolution of symptoms :patient was normal 8 months back then developed b/l pedal edema which gradually progressed.
Aggerevated in sitting and standing position, relived on taking medication
*Palpitations :since 5days, sudden in onset which is more during night
Aggerevated by lifting heavy weights, speaking continuously
*Dyspnoea during palpitations (NYHA-3) since 5 days
pain:since 6days, radiating along left upper limb, more during palpitations and relived on medication.
Chest pain associated with chest heaviness since 5 days
Anatomical localisation :
Palpitations
Dyspnoea(NYHA-3)

Pedal edema
Chest pain
Etiological agent :
*By localization, electrolyte imbalance (hypokalemia) causing the her manifestations like palpitations, chest heaviness, generalised body weak ness
*radiating pain along her left upper limb due to cervical spondylosis.
2Q)What are the reasons for recurrence of hypokalemia in her? Important risk factors for her hypokalemia?
A) Reason: recurrent hypokalemic periodic paralysis
Current risk factor:due to use of diuretics
Other risk factors
A) Abnormal loses:
Medications-diuretics, laxatives, enema, corticosteriods
Real causes- osmotic diuresis, mineralo corticoid excess, renal tubular acidosis, hypomagnesenemia
B) trance cellular shift : alkalosis, thyrotoxicosis, delirium tremans, head injury, Myocardial, ischemia, recurrent hypokalemic periodic paralysis
C) Inadequate intake: anorexia, dementia, stareation, total parental nutrition
D) psuedohypokalemia:delayed sample analysis, significant leukocytosis
3) What are the changes seen in ECG in case of hypokalemia and associated symptoms?
changes seen in ECG :
A)Earliest change :decreased T-wave amplitude, ST depression, Twave - and inversion or flat;prolonged PR interval;presence of Uwaves
In Severe cases :ventricular fibrillation, rarely AV block .
Symptoms of hypokalemia:
Weakness & fatigue, palpitations, muscle cramps & pain, anxiety, psychosis, depression, delirium.
D) Link to patient details:
https://rishikoundinya.blogspot.com/2021/05/55years-old-patient-with-seizures.htm
Questions:
1.Is there any relationship between occurrence of seizure to brain stroke. If yes what is the mechanism behind it?
seizures after ischaemic strokes. An increase in intracellular Ca2+ and Na+ with a resultant lower threshold for depolarisation, glutamate excitotoxicity, hypoxia, metabolic dysfunction, global hypoperfusion, and hyperperfusion injury
Seizures after haemorrhagic strokes are thought to be attributable to irritation due to (hemosideri. Deposits)caused by products of blood metabolism
Late onset seizures are associated with the persistent changes in neuronal excitability and gliotic scarring is most probably the underlying cause.
2. In the previous episodes of seizures, patient didn't loose his consciousness but in the recent episode he lost his consciousness what might be the reason?
Initially the patient might have had Simple partial seizures (no loss of consciousness) and might have progressed to Generalised Tonic Clonic seizures (loss of consciousness)
E) Link to patient details:
https://nikhilasampathkumar.blogspot.com/2021/05/a-48-year-old-male-with-seizures-and.html?m=1
Questions: 1) What could have been the reason for this patient to develop ataxia in the past 1 year?
The patient has minor unattended head injuries in the past 1 yr. Accoding to the CT scan, the patient has cerebral haemorrhage in the frontal lobe causing probably for the occurrence of Frontal love ataxia
2) What was the reason for his IC bleed? Does Alcoholism contribute to bleeding diatheses ?
The patient has minor unattended head injuries. During the course of time the minor hemorrhages if present should have been cured on their own. But the patient is a chronic alcholic. This might have hindered the process of healing or might have stopped the healing rendering it to grow further more into 13 mm sized hemorrhages occupying Frontal Parietal and Temporal lobes
F) Link to patient details:
http://shivanireddymedicalcasediscussion.blogspot.com/2021/05/a-30-yr-old-male-patient-with-weakness.html
Questions
1.Does the patient's history of road traffic accident have any role in his present condition?
The closeness of facial bones to the cranium would suggest that there are chances of cranial injuries. Since the Zygomatic arch and Mandibular process is very close to the cranium, this might play a role in the patient's present condition
2.What are warning signs of CVA?
Weakness or numbness of the face, arm or leg, usually on one side of the body
Trouble speaking or understanding
Problems with vision, such as dimness or loss of vision in one or both eyes
Dizziness or problems with balance or coordination
Problems with movement or walking
Fainting or seizure
Severe headaches with no known cause, especially if they happen suddenly
3.What is the drug rationale in CVA?
Mannitol- Because of its osmotic effect, mannitol is assumed to decrease cerebral edema. Mannitol might improve cerebral perfusion by decreasing viscosity, and as a free-radical scavenger, it might act as a neuroprotectant.
Ecospirin
For the prevention of heart attack, stroke, heart conditions such as stable or unstable angina (chest pain) due to a blood clot.
Atrovas-Atorva 40 Tablet belongs to a group of medicines called statins. It is used to lower cholesterol and to reduce the risk of heart diseases. Cholesterol is a fatty substance that builds up in your blood vessels and causes narrowing, which may lead to a heart attack or stroke.
Rt feed RT feed is a nursing procedure to provide nutrition to those people who are either unable to obtain nutrition by mouth or are not in a state to swallow the food safely.
4. Does alcohol has any role in his attack?
When the patient met with an accident there might be cranial damage which was unnoticed.
If so his occasional drinking may or may not have hindered the process of the minor hemorrhages getting healed and might have caused this condition
But since the patient is not a chronic alcoholic and so Alcohol might not have played any role.
Therefore it cannot be evaluated without further details
5.Does his lipid profile has any role for his attack??
The inverse relationship between serum HDL-C and stroke risk . When taken together it seems clear that higher baseline levels of serum HDL-C lower the risk of subsequent ischemic stroke.
G)Link to patient details:
https://amishajaiswal03eloggm.blogspot.com/2021/05/a-50-year-old-patient-with-cervical.html
Questions:
1)what is myelopathy hand?There is loss of power of adduction and extension of the ulnar two or three fingers and an inability to grip and release rapidly with these fingers. These changes have been termed "myelopathy hand" and appear to be due to pyramidal tract involvement.
2)what is finger escape?
Finger escape
Wartenberg's sign is a neurological sign consisting of involuntary abduction of the fifth (little) finger, caused by unopposed action of the extensor digiti minimi. . This finding of weak finger adduction in cervical myelopathy is also called the "finger escape sign".
3)what is Hoffman's sign?
Hoffman's sign or reflex is a test used to examine the reflexes of the upper extremities. This test is a quick, equipment-free way to test for the possible existence of spinal cord compression from a lesion on the spinal cord or another underlying nerve condition
H)Link to patient details:
https://neerajareddysingur.blogspot.com/2021/05/general-medicine-case-discussion.html?m=1
A 17 year old female student by occupation presented to causality on 1/5/2021 with
Chief complaints of
1.Involuntary movements of both upper and lower limbs a day before.
Questions:
1) What can be the cause of her condition ?
According to MRI cortical vein thrombosis might be the cause of her seizures.
2) What are the risk factors for cortical vein thrombosis?
Infections:
Meningitis, otitis,mastoiditis
Prothrombotic states:
Pregnancy, puerperium,antithrombin deficiency proteinc and protein s deficiency,Hormone replacement therapy.
Mechanical:
Head trauma,lumbar puncture
Inflammatory:
SLE,sarcoidosis,Inflammatory bowel disease.
Malignancy.
Dehydration
Nephrotic syndrome
Drugs:
Oral contraceptives,steroids,Inhibitors of angiogenesis
Chemotherapy:Cyclosporine and l asparginase
Hematological:
Myeloproliferative Malignancies
Primary and secondary polycythemia
Intracranial :
Dural fistula,
venous anomalies
Vasculitis:
Behcets disease wegeners granulomatosis
3)There was seizure free period in between but again sudden episode of GTCS why?resolved spontaneously why?
Seizures are resolved and seizure free period got achieved after medical intervention but sudden episode of seizure was may be due to any persistence of excitable foci by abnormal firing of neurons.
4) What drug was used in suspicion of cortical venous sinus thrombosis?
Anticoagulants are used for the prevention of harmful blood clots.
Clexane ( enoxaparin) low molecular weight heparin binds and potentiates antithrombin three a serine protease Inhibitor to form complex and irreversibly inactivates factor xa.
3) CARDIOLOGY:
A)Link to patient details:
https://muskaangoyal.blogspot.com/2021/05/a-78year-old-male-with-shortness-of.html
A 78 yr old male patient, resident of of kattangur and shepherd by occupation came to the Opd on 14 /5/2021 with chief complaints of :
SHORTNESS OF BREATH ,SINCE 20 DAYS
CHEST PAIN ,SINCE 20 DAYS
B/L PEDAL EDEMA , SINCE 4 DAYS
FACIAL PUFFINESS , SINCE 4 DAYS
Questions:
1.What is the difference btw heart failure with preserved ejection fraction and with reduced ejection fraction?
Ans:Preserved ejection fraction (HFpEF) – also referred to as diastolic heart failure. The heart muscle contracts normally but the ventricles do not relax as they should during ventricular filling (or when the ventricles relax).
Reduced ejection fraction (HFrEF) – also referred to as systolic heart failure
HFpEF is preceded by chronic comorbidities, such as hypertension, type 2 diabetes mellitus (T2DM), obesity, and renal insufficiency, whereas HFrEF is often preceded by the acute or chronic loss of cardiomyocytes due to ischemia, a genetic mutation, myocarditis, or valvular disease
2.Why haven't we done pericardiocenetis in this pateint?
Ans: Pericardiocentesis is not done here Because the effusion was self healing ,It reduced from 2.4cm to 1.9 cm.
3.What are the risk factors for development of heart failure in the patient?
Ans: risk factors for development of heart faliure in this patent
Alcohol abuse increases the risk of atrial fibrillation, heart attack and congestive heart failure
high blood pressure
Smoking
Diabetes
AV block can be associated with severe bradycardia and hemodynamic instability. It has a greater risk of progressing to third-degree (complete) heart block or asystole.
wosening of pericardial effusion leaing to cardiac tamponade.
4.What could be the cause for hypotension in this
Ans : visceral pericardium may have thickened which is restricting the heart to expand causing hypotension
(May be secondary to TB)
B)Link to patient details:
https://muskaangoyal.blogspot.com/2021/05/a-73-year-old-male-patient-with-pedal.html
QUESTION: What are the possible causes for heart failure in this patient?
the patient has various comorbidities which could have led to a heart failure
1. The patient was diagnosed with type 2 diabetes mellitus 30 years ago and has been taking human mixtrad insulin daily and was also diagnosed with diabetic triopathy indicating uncontrolled diabetes which is major risk factor for heart failure
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5494155/
2. The patient was also diagnosed with hypertension 19 yrs. ago which is also a risk factor for heart failure
https://pubmed.ncbi.nlm.nih.gov/31472888/
3. He is a chronic alcoholic since 40 years which is a risk factor towards heart failure
https://www.nmcd-journal.com/article/S0939-4753(19)30360-6/fulltext
The findings in this article provide longitudinal evidence that moderate and heavy alcohol consumption are associated with decreased LVEF and trend towards a higher risk of incident LV systolic dysfunction, compared to light drinkers.
4. The patient has elevated creatinine and AST/ALT ratios is >2 and was diagnosed with chronic kidney disease stage IV. CKD is also one of the risk factors for heart failure
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2900793/
QUESTION: what is the reason for anaemia in this case?
The patient has normocytic normochromic anaemia. it could be anaemia of a chronic disease as the patient is diagnosed with CKD stage IV.
Chronic kidney disease results in decreased production of erythropoietin which in turn decreases the production of red blood cells from the bone marrow.
Patient’s with anaemia and CKD also tend to have deficiency in nutrients like iron, vitamin B12 and folic acid essential in making healthy red blood cells
QUESTION: What is the reason for blebs and non-healing ulcer in the legs of this patient?
The most common cause for blebs and non-healing ulcer in this patient is diabetes mellitus. CKD is also known to cause delay in healing of wounds along with poorly controlled diabetes. Anaemia can also slow down the process of healing due to low oxygen levels.
QUESTION: What sequence of stages of diabetes has been noted in this patient?
There are 4 stages in type 2 diabetes- insulin resistance, prediabetes, type 2 diabetes and type 2 diabetes and vascular complications, including retinopathy, nephropathy or neuropathy and, or, related microvascular events.
The patient is diagnosed with diabetic triopathy exhibiting sequence of neuropathy, retinopathy and nephropathy
The patient has been diagnosed with diabetic retinopathy, CKD stage IV and shows signs of diabetic neuropathy such as numbness
C) Link to patient details:
https://preityarlagadda.blogspot.com/2021/05/biatrial-thrombus-in-52yr-old-male.html
A 52yr old male came to the OPD with the chief complaints of decreased urine output and shortness of breath at rest since one day.
Questions:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Ans: *the anatomical site is BLOOD VESSELS;
* ETIOLOGY:
The physical stress of hypertension on the arterial wall also results in the aggravation and acceleration of atherosclerosis, particularly of the coronary and cerebral vessels. Moreover, hypertension appears to increase the susceptibility of the small and large arteries to atherosclerosis.
The most likely cause of arterial thrombosis is artery damage due to atherosclerosis. Atherosclerosis occurs when a person has a buildup of plaque on the walls of their arteries. The arteries then begin to narrow and harden, which increases a person's risk of developing arterial thrombosis.
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
Ans: PHARMACOLOGICAL INTERVENTIONS
1. TAB. Dytor
mechanism: Through its action in antagonizing the effect of aldosterone, spironolactone inhibits the exchange of sodium for potassium in the distal renal tubule and helps to prevent potassium loss.
2. TAB. Acitrom
mechanism: Acenocoumarol inhibits the action of an enzyme Vitamin K-epoxide reductase which is required for regeneration and maintaining levels of vitamin K required for blood clotting
3. TAB. Cardivas
mechanism:Carvedilol works by blocking the action of certain natural substances in your body, such as epinephrine, on the heart and blood vessels. This effect lowers your heart rate, blood pressure, and strain on your heart. Carvedilol belongs to a class of drugs known as alpha and beta-blockers.
4. INJ. HAI S/C
MECHANISM:Regulates glucose metabolism
Insulin and its analogues lower blood glucose by stimulating peripheral glucose uptake, especially by skeletal muscle and fat, and by inhibiting hepatic glucose production; insulin inhibits lipolysis and proteolysis and enhances protein synthesis; targets include skeletal muscle, liver, and adipose tissue
5.TAB. Digoxin
mechanism:
Digoxin has two principal mechanisms of action which are selectively employed depending on the indication:
Positive Ionotropic: It increases the force of contraction of the heart by reversibly inhibiting the activity of the myocardial Na-K ATPase pump,
an enzyme that controls the movement of ions into the heart.
6. Hypoglycemia symptoms explained
7. Watch for any bleeding manifestations like Petechiae, Bleeding gums.
8. APTT and INR are ordered on a regular basis when a person is taking the anticoagulant drug warfarin to make sure that the drug is producing the desired effect.
3) What is the pathogenesis of renal involvement due to heart failure (cardio renal syndrome)? Which type of cardio renal syndrome is this patient?
Ans: *cardiorenal syndrome type 4 is seen in this patient.
4) What are the risk factors for atherosclerosis in this patient?
Ans: effect of hypertention
They can also impair blood vessels' ability to relax and may stimulate the growth of smooth muscle cells inside arteries. All these changes can contribute to the artery-clogging process known as atherosclerosis.
5) Why was the patient asked to get those APTT, INR tests for review?
Ans: APTT and INR are ordered on a regular basis when a person is taking the anticoagulant drug warfarin to make sure that the drug is producing the desired effect.
Here, an INR of 3-4.5 is recommended. Warfarin should be started in conjunction with heparin or low molecular weight heparin when the diagnosis of venous thromboembolism is confirmed, although local protocols may vary in their starting doses and titration schedule.
D)Link to patient details:
https://daddalavineeshachowdary.blogspot.com/2021/05/67-year-old-patient-with-acute-coronary.html?m=1
Questions:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
TIMELINE OF EVENTS-
• Diabetes since 12 years - on medication
• Heart burn like episodes since an year- relieved without medication
• Diagnosed with pulmonary TB 7 months ago- completed full course of treatment, presently sputum negative.
• Hypertension since 6 months - on medication
• Shortness of breath since half an hour-SOB even at rest
Anatomical localisation - Cardiovascular system
Etiology: The patient is both Hypertensive and diabetic , both these conditions can cause
- Atherosclerosis: there is build up of fatty and fibrous material inside the wall of arteries.(PLAQUE)
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
Pharmacological interventions:
TAB MET XL 25 MG/STAT-contains Metoprolol as active ingredient
MOA: METOPROLOL is a cardiselective beta blocker
Beta blockers work by blocking the effects of the hormone epinephrine, also known as adrenaline. Beta blockers cause your heart to beat more slowly( negative chronotropic effect)
and with less force( negative inotropic effect). Beta blockers also help open up your veins and arteries to improve blood flow.
Indications: it is used to treat Angina, High blood pressure and to lower the risk of hear attacks .
EFFICACY STUDIES.
Patients were randomized to one of four treatment arms: placebo or ER metoprolol (0.2 mg/kg, 1.0 mg/kg, or 2.0 mg/kg). Data were analyzed on 140 intent-to-treat patients.
Results: mean baseline BP was 132/78 +/- 9/9 mmHg. Following 4 weeks of treatment, mean changes in sitting BP were: placebo = -1.9/-2.1 mmHg; ER metoprolol 0.2 mg/kg = -5.2/-3.1 mmHg; 1.0 mg/kg = -7.7/-4.9 mmHg; 2.0 mg/kg = -6.3/-7.5 mmHg. Compared with placebo, ER metoprolol significantly reduced systolic blood pressure (SBP) at the 1.0 and 2.0 mg/kg dose (P = .027 and P = .049, respectively), reduced diastolic blood pressure (DBP) at the 2.0 mg/kg dose (P = .017), and showed a statistically significant dose response relationship for the placebo-corrected change in DBP from baseline. There were no serious adverse events or adverse events requiring study drug discontinuation among patients receiving active therapy.
Non pharmacological intervention advised to this patient is: PERCUTANEOUS CORONARY INTERVENTION.
Percutaneous Coronary Intervention is a non-surgical procedure that uses a catheter (a thin flexible tube) to place a small structure called a stent to open up blood vessels in the heart that have been narrowed by plaque buildup ( atherosclerosis).
3) What are the indications and contraindications for PCI?
INDICATIONS:
Acute ST-elevation myocardial infarction (STEMI)
Non–ST-elevation acute coronary syndrome (NSTE-ACS)
Unstable angina.
Stable angina.
Anginal equivalent (eg, dyspnea, arrhythmia, or dizziness or syncope)
High risk stress test findings.
CONTRAINDICATIONS:
Intolerance for oral antiplatelets long-term.
Absence of cardiac surgery backup.
Hypercoagulable state.
High-grade chronic kidney disease.
Chronic total occlusion of SVG.
An artery with a diameter of <1.5 mm.
4) What happens if a PCI is performed in a patient who does not need it? What are the harms of overtreatment and why is research on overtesting and overtreatment important to current healthcare systems?
Although PCI is generally a safe procedure , it might cause serious certain complications like
A)Bleeding
B) Blood vessel damage
C) Allergic reaction to the contrast dye used
D) Arrhythmias
E) Need for emergency coronary artery bypass grafting .
Because of all these complications it is better to avoid PCI in patients who do not require it.
⁃ OVER TESTING AND OVER TRAETMENT HAVE BECOME COMMMIN IN TODAY’S MEDICAL PRACTICE.
⁃ Research on overtesting and overtreatment is important as they are more harmful than useful.
Harms to patients
. Performing screening tests in patients with who at low risk for the disease which is being screened.
For example:Breast Cancer Screenings Can Cause More Harm Than Good in Women Who Are at Low Risk. A harmless lump or bump could incorrectly come up as cancer during routine breast screenings. This means that some women undergo surgery, chemotherapy or radiation for cancer that was never there in the first place.
.Overuse of imaging techniques such as X- RAYS AND CT SCANS as a part of routine investigations.
Overuse of imaging can lead to a diagnosis of a condition that would have otherwise remained irrelevant - OVERDIAGNOSIS.
Also the adverse effects due to this are more when compared to the benefits.
.Overdiagnosis through overtesting can psychologically harm the patient.
Hospitalizations[41] for those with chronic conditions who could be treated as outpatients[ can lead to economic burden and a feeling of isolation.
Harms to health care systems
The use of expensive technologies and machineries are causing burden on health care systems.
E) Link to patient details:
https://bhavaniv.blogspot.com/2021/05/case-discussion-on-myocardial-infarction.html?m=1
Questions:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
TIMELINE OF EVENTS-
• Diabetes since 12 years - on medication
• Heart burn like episodes since an year- relieved without medication
• Diagnosed with pulmonary TB 7 months ago- completed full course of treatment, presently sputum negative.
• Hypertension since 6 months - on medication
• Shortness of breath since half an hour-SOB even at rest
Anatomical localisation - Cardiovascular system
Etiology: The patient is both Hypertensive and diabetic , both these conditions can cause
- Atherosclerosis: there is build up of fatty and fibrous material inside the wall of arteries.(PLAQUE)
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
Pharmacological interventions:
TAB MET XL 25 MG/STAT-contains Metoprolol as active ingredient
MOA: METOPROLOL is a cardiselective beta blocker
Beta blockers work by blocking the effects of the hormone epinephrine, also known as adrenaline. Beta blockers cause your heart to beat more slowly( negative chronotropic effect)
and with less force( negative inotropic effect). Beta blockers also help open up your veins and arteries to improve blood flow.
Indications: it is used to treat Angina, High blood pressure and to lower the risk of hear attacks .
EFFICACY STUDIES.
Patients were randomized to one of four treatment arms: placebo or ER metoprolol (0.2 mg/kg, 1.0 mg/kg, or 2.0 mg/kg). Data were analyzed on 140 intent-to-treat patients.
Results: mean baseline BP was 132/78 +/- 9/9 mmHg. Following 4 weeks of treatment, mean changes in sitting BP were: placebo = -1.9/-2.1 mmHg; ER metoprolol 0.2 mg/kg = -5.2/-3.1 mmHg; 1.0 mg/kg = -7.7/-4.9 mmHg; 2.0 mg/kg = -6.3/-7.5 mmHg. Compared with placebo, ER metoprolol significantly reduced systolic blood pressure (SBP) at the 1.0 and 2.0 mg/kg dose (P = .027 and P = .049, respectively), reduced diastolic blood pressure (DBP) at the 2.0 mg/kg dose (P = .017), and showed a statistically significant dose response relationship for the placebo-corrected change in DBP from baseline. There were no serious adverse events or adverse events requiring study drug discontinuation among patients receiving active therapy.
Non pharmacological intervention advised to this patient is: PERCUTANEOUS CORONARY INTERVENTION.
Percutaneous Coronary Intervention is a non-surgical procedure that uses a catheter (a thin flexible tube) to place a small structure called a stent to open up blood vessels in the heart that have been narrowed by plaque buildup ( atherosclerosis).
3) What are the indications and contraindications for PCI?
INDICATIONS:
Acute ST-elevation myocardial infarction (STEMI)
Non–ST-elevation acute coronary syndrome (NSTE-ACS)
Unstable angina.
Stable angina.
Anginal equivalent (eg, dyspnea, arrhythmia, or dizziness or syncope)
High risk stress test findings.
CONTRAINDICATIONS:
Intolerance for oral antiplatelets long-term.
Absence of cardiac surgery backup.
Hypercoagulable state.
High-grade chronic kidney disease.
Chronic total occlusion of SVG.
An artery with a diameter of <1.5 mm.
4) What happens if a PCI is performed in a patient who does not need it? What are the harms of overtreatment and why is research on overtesting and overtreatment important to current healthcare systems?
Although PCI is generally a safe procedure , it might cause serious certain complications like
A)Bleeding
B) Blood vessel damage
C) Allergic reaction to the contrast dye used
D) Arrhythmias
E) Need for emergency coronary artery bypass grafting .
Because of all these complications it is better to avoid PCI in patients who do not require it.
⁃ OVER TESTING AND OVER TRAETMENT HAVE BECOME COMMMIN IN TODAY’S MEDICAL PRACTICE.
⁃ Research on overtesting and overtreatment is important as they are more harmful than useful.
Harms to patients
. Performing screening tests in patients with who at low risk for the disease which is being screened.
For example:Breast Cancer Screenings Can Cause More Harm Than Good in Women Who Are at Low Risk. A harmless lump or bump could incorrectly come up as cancer during routine breast screenings. This means that some women undergo surgery, chemotherapy or radiation for cancer that was never there in the first place.
.Overuse of imaging techniques such as X- RAYS AND CT SCANS as a part of routine investigations.
Overuse of imaging can lead to a diagnosis of a condition that would have otherwise remained irrelevant - OVERDIAGNOSIS.
Also the adverse effects due to this are more when compared to the benefits.
.Overdiagnosis through overtesting can psychologically harm the patient.
Hospitalizations[41] for those with chronic conditions who could be treated as outpatients[ can lead to economic burden and a feeling of isolation.
Harms to health care systems
The use of expensive technologies and machineries are causing burden on health care systems.
F) Link to patient details:
https://kattekolasathwik.blogspot.com/2021/05/a-case-of-cardiogenic-shock.h
Questions:
1. How did the patient get relieved from his shortness of breath after i.v fluids administration by rural medical practitioner?
Because of the fluid loss occurred to the patient
there is decreased preload- so, SOB occurred due to decreased CO
IV fluids administered- there is increased preload- SOB decreased due to better of cardiac output.
2. What is the rationale of using torsemide in this patient?
Torsemide used to relieve abdominal distension.
3. Was the rationale for administration of ceftriaxone? Was it prophylactic or for the treatment of UTI?
IT IS THE TREATMENT FOR UTI
Rationale- Used for any bacterial infection.
4)Gastroenterology (& Pulmonology) 10 Marks
A) Link to patient details:
https://63konakanchihyndavi.blogspot.com/2021/05/case-discussion-on-pancreatitis-with.html
QUESTIONS:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Evolution of symptomatology
H5 years back-1st episode of pain abdomen and vomitings
Stopped taking alcohol for 3 years
1 year back 5 to 6 episodes of pain abdomen and vomitings after starting to drink alcohol again
20 days back increased consumption of toddy intake
Since 1 week pain abdomen and vomiting
Since 4 days fever constipation and burning micturition
Anatomical localisation: Pancreas and left lung
Alcohol and its metabolites produce changes in the acinar cells, which may promote premature intracellular digestive enzyme activation thereby predisposing the gland to autodigestive injury. Pancreatic stellate cells (PSCs) are activated directly by alcohol and its metabolites and also by cytokines and growth factors released during alcohol-induced pancreatic necroinflammation. Activated PSCs are the key cells responsible for producing the fibrosis of alcoholic chronic pancreatitis
2) What is the efficacy of drugs used along with other non pharmacological treatment modalities and how would you approach this patient as a treating physician?
1) ING. MEROPENAM ; TID for 7 days
* Meropenem ( broad spectrum Carbepenem ) an antibiotic.
2) ING. METROGYL 500 mg IV TID for 5 days
* inj. Metrogyl has METRONIDAZOLE
( Nitroimidazole drug ) an antibiotic
3) ING. AMIKACIN 500 mg IV BD for 5days
* It is an Aminoglycoside antibiotic
## Here all three of these (Inj. Meropenem, Inj. Metrogyl, Inj. Amikacin ) are used as antibiotics to control infection and ; to prevent septic complications of acute pancreatitis.
4) TPN ( Total Parenteral Nutrition )
* Method of feeding that by passes gastrointestinal tract
* Fluids are given to vein , it provides most of the nutrients body needs.
* TPN has proteins, carbohydrates, fats, vitamins, minerals.
5) IV NS / RL at the rate 12l ml per hour
* Given for fluid replacement ie., treat dehydration
6) ING. OCTREOTIDE 100 mg SC , BD
* It is a Somatostatin long acting analogue.
* It is used here to decrease exocrine secretion of pancreas and it also has anti- inflammatory & cytoprotective effects.
7) ING. PANTOP 40 mg IV , OD
* Inj. Pantop has PANTOPRAZOLE ( Proton Pump Inhibitor) used for its anti pancreatic secretory effect.
8) ING. THIAMINE 100 mg in 100 ml NS IV , TID
* It is B1 supplement.
* It is given here because; due to long fasting & TPN usage , body may develop B1 deficiency
* Wernicke encephalopathy secondary to B1 deficiency may be caused... so a prophylactic B1 supplemention is necessary.
9) ING. TRAMADOL in 100 ml NS IV , OD
* It is an opioid analgesic, given to releive pain
B) Link to patient details:
https://nehae-logs.blogspot.com/2021/05/case-discussion-on-25-year-old-male.html
Questions:
a)the cause of dyspnea might be PLEURAL EFFUSION
b)
*This hyperglycemia could thus be the result of a hyperglucagonemia secondary to stress
* the result of decreased synthesis and release of insulin secondary to the damage of pancreatic β-cells
* elevated levels of catecholamines and cortisol
c)
LFT are increased due to hepatocyte injury
*If the liver is damaged or not functioning properly, ALT can be released into the blood. This causes ALT levels to increase. A higher than normal result on this test can be a sign of liver damage.
*elevated alanine transaminase (ALT) and aspartate transaminase (AST), usually one to four times the upper limits of normal in alcoholic fatty liver.
The reasons for a classical 2:1 excess of serum AST activity compared to serum ALT activity in alcoholic hepatitis have been attributed to
(i) decreased ALT activity most likely due to B6 depletion in the livers of alcoholics
(ii) mitochondrial damage leading to increased release of mAST in serum.
d)
Plan of action and Treatment:
Investigations:
✓ 24 hour urinary protein
✓ Fasting and Post prandial Blood glucose
✓ HbA1c
✓ USG guided pleural tapping
Treatment:
• IVF: 125 mL/hr
• Inj PAN 40mg i.v OD
• Inj ZOFER 4mg i.v sos
• Inj Tramadol 1 amp in 100 mL NS, i.v sos
• Tab Dolo 650mg sos
• GRBS charting 6th hourly
• BP charting 8th hourly
C)Link to patient details:
https://chennabhavana.blogspot.com/2021/05/general-medicine-case-discussion-1.html
Questions:
What is the most probable diagnosis in this patient?
àDifferential Diagnosis:
• Ruptured Liver Abscess.
• Organized collection secondary to Hollow viscous Perforation.
• Organized Intraperitoneal Hematoma.
• Free fluid with internal echoes in Bilateral in the Subdiaphragmatic space.
• Grade 3 RPD of right Kidney
àThe most probably diagnosis is there is abdominal hemorrhage. This will give reasoning to the abdominal distention, and the blood which is aspirated.
2) What was the cause of her death?
àAfter leaving the hospital, the patient went to Hyderabad and underwent an emergency laparotomy surgery. The patient passed away the next day. Cause of her death can be due to complications of laparotomy surgery such as, hemorrhage (bleeding), infection, or damage to internal organs.
3) Does her NSAID abuse have something to do with her condition? How?
àNSAID-induced renal dysfunction has a wide spectrum of negative effects, including decreased glomerular perfusion, decreased glomerular filtration rate, and acute renal failure. Chronic NSAIDs use has also been related to hepatotoxicity. While the major adverse effects of NSAIDs such as gastrointestinal mucosa injury are well known, NSAIDs have also been associated with hepatic side effects ranging from asymptomatic elevations in serum aminotransferase levels and hepatitis with jaundice to fulminant liver failure and death.
5) NEPHROLOGY(and UROLOGY)
A)Link to patient details:
https://kavyasamudrala.blogspot.com/2021/05/medicine-case-discussion-this-is-online.html
Questions:
1.what could be the cause for his SOB
Ans- His sob was is due to Acidosis which was caused by Diuretics
2. Reason for Intermittent Episodes of drowsiness
Ans-Hyponatremia was the cause for his drowsiness
3.why did he complaint of fleshy mass like passage inurine
Ans-plenty of pus cells in his urine passage appeared as
fleshy mass like passage to him
4. What are the complicat ions of TURP that he may have had
Ans-
Difficulty micturition
Electrolyte imbalances
Infection
B)Link to patient details:
https://drsaranyaroshni.blogspot.com/2021/05/an-eight-year-old-with-frequent.html
Questions
1.Why is the child excessively hyperactive without much of social etiquettes ?
Attention deficit hyperactivity disorder (ADHD) is a neurodevelopmental disorder characterized by inattention, or excessive activity and impulsivity, which are otherwise not appropriate for a person's age
For a diagnosis, the symptoms have to be present for more than six months, and cause problems in at least two settings (such as school, home, work, or recreational activities).
2. Why doesn't the child have the excessive urge of urination at night time ?
Since the child doesn’t have excessive urge of urination at night but at day there might be a psychiatry related condition
1. Psychosomatic disorder
2. Undiagnosed anxiety disorder
3. How would you want to manage the patient to relieve him of his symptoms?
bacterial kidney infection, the typical course of treatment is antibiotic and painkiller therapy.
If the cause is an overactive bladder, a medication known as an anticholinergic may be used. These prevent abnormal involuntary detrusor muscle contractions from occurring in the wall of the bladder
To treat attention deficit hyperactivity disorder:
For children 6 years of age and older, the recommendations include medication and behavior therapy together — parent training in behavior management for children up to age 12 and other types of behavior therapy and training for adolescents. Schools can be part of the treatment as well.
Methylphenidate A stimulant and a medication used to treat Attention Deficit Hyperactivity Disorder. It can make you feel very ‘up’, awake, excited, alert and energised, but they can also make you feel agitated and aggressive. They may also stop you from feeling hungry.
Amphetamine belongs to a class of drugs known as stimulants. It can help increase your ability to pay attention, stay focused on an activity, and control behavior problems. It may also help you to organize your tasks and improve listening skills.
6)Infectious Disease (HI virus, Mycobacteria, Gastroenterology, Pulmonology) 10 Marks
A) Link to patient details:
https://vyshnavikonakalla.blogspot.com/2021/05/a-40-year-old-lady-with-dysphagia-fever.html
QUESTION 1:
1.Which clinical history and physical findings are characteristic of tracheo esophageal fistula?
ANSWER:
Clinical history:
Cough since 2 months on taking food and liquids
•difficulty in swallowing since 2 month . It was initially difficult only with solids but then followed by liquids also.
•hoarseness of voice,sob in later stages
Physical findings:
Weight loss
Pallor
Respiratory system: wheeze and diffuse crepts
Aspiration
Spo2 decreased on room air
CBP:Hbpercent decreased
RVD positive likely to develop tracheo -esophageal fistula
These favour for tracheo esophageal.fistula
QUESTION 2:
2) What are the chances of this patient developing immune reconstitution inflammatory syndrome? Can we prevent it?
ANSWER:
Immune reconstitution inflammatory syndrome (IRIS) represents the worsening of a recognized (paradoxical IRIS) or unrecognized (unmasking IRIS) pre-existing infection in the setting of improved immunologic function.
The most effective prevention of IRIS would involve initiation of ART before the development of advanced immunosuppression. IRIS is uncommon in individuals who initiate antiretroviral treatment with a CD4+ T-cell count greater than 100 cells/uL.
Aggressive efforts should be made to detect asymptomatic mycobacterial or cryptococcal disease prior to the initiation of ART, especially in areas endemic for these pathogens and with CD4 T-cell counts less than 100 cells/uL.
Two prospective randomized studies are evaluating prednisone and meloxicam for the prevention of paradoxical TB IRIS.
7)Infectious disease and Hepatology:
A)Link to patient details:
https://kavyasamudrala.blogspot.com/2021/05/liver-abscess.html
Liver abscess
1Q)do u think drinking locally made alcohol cause liver abscess in this patient due to predisposing factors present in it ? What could be the cause in this patient?
1ans- yes, it could be due to intake of contaminated toddy
2Q)what is the etiopathogenesis of liver abscess in a chronic alcoholic patient?(since 30 yrs - 1 bottle/day)
2ans - according to some studies, alcoholism mainly consuming locally prepared alcohol plays a major role as a predisposing factor for the formation of liver abscesses that is both amoebic as well as pyogenic liver abscess because of the adverse effects of alcohol over the Liver. It is also proven that Alcoholism is never an etiological factor for the formation of liver abscess.
3Q)is liver abscess is more common in right lobe?
3ans-yes right lobe is involved due to its moreblood supply
4Q) what r the indications for usg guided aspiration of liver abscess
4ans- Indications for USG guided aspiration of liver abscess
1. Large abscess more than 6cms
2. Left lobe abscess
3.Caudate lobe abscess
4. Abscess which is not responding to drugs
B)Link to patient details:
https://63konakanchihyndavi.blogspot.com/2021/05/case-discussion-on-liver-abcess.html
1) Cause of liver abcess in this patient ?
A) Here ; the cause of liver abcess is :
* Amoebic liver abcess (ALA ) seen commonly in the tropics is predominantly confined to adult males, especially those who consume locally brewed alcohol, although intestinal amoebiasis occurs in all age groups and in both genders.
* It has been argued that socioeconomic factors and poor sanitary conditions are the primary culprits that casually link alcohol to ALA.
* However , there has emerged an abundance of data that implicates alcohol in a more causal role in facilitating the extraintestinal invasion of the infective protozoan and the subsequent development of ALA.
## Hence the consumption of locally made alcohol ( toddy ) is the most likely cause of Liver abcess in this patient.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6077556/
2) How do you approach this patient ?
A) * The patient is well managed by treating team ; even me will follow the same approach.
3) Why do we treat here ; both amoebic and pyogenic liver abscess?
A) * Considering the following factors:
1) Age and gender of patient: 21 years ( young ) and male.
2) Single abcess.
3) Right lobe involvement.
## The abcess is most likely AMOEBIC LIVER ABSCESS …
** But most of the patients with amoebic liver abcess have no bowel symptoms, examination of stool for ova and parasite and antigen testing is insensitive and insensitive and not recommended.
# And considering the risk factors associated with aspiration for pus culture:
1) Sometimes ; abcess is not accessible for aspiration if it is in posterior aspect or so.
2) Sometimes ; it has thin thinwall which may rupture if u aspirate.
3) Sometimes ; it is unliquefied.
## There how can u confirm whether it is pyogenic/ amoebic , so we treat them both empirically in clinical practice.
https://academic.oup.com/bmb/article/132/1/45/5677141
4) Is there a way to confirmthe definitive diagnosis in this patient?
A) There is no way to confirm the definitive diagnosis…(as mentioned above)
8)Infectious disease (Mucormycosis, Ophthalmology, Otorhinolaryngology, Neurology) 10 Marks
A) Link to patient details:
http://manikaraovinay.blogspot.com/2021/05/50male-came-in-altered-sensorium.html
QUESTION: What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary aetiology of the patient's problem?
1. 3 years ago- diagnosed with hypertension
2. 21 days ago- received vaccination at local PHC which was followed by fever associated with chills and rigors, high grade fever, no diurnal variation which was relieved on medication
3. 18 days ago- complained of similar events and went to the the local hospital, it was not subsided upon taking medication(antipyretics)
4. 11 days ago - c/o Generalized weakness and facial puffiness and periorbital oedema. Patient was in a drowsy state
5. 4 days ago-
a. patient presented to casualty in altered state with facial puffiness and periorbital oedema and weakness of right upper limb and lower limb
b. towards the evening patient periorbital oedema progressed
c. serous discharge from the left eye that was blood tinged
d. was diagnosed with diabetes mellitus
6. patient was referred to a government general hospital
7. patient died 2 days ago
patient was diagnosed with diabetic ketoacidosis and was unaware that he was diabetic until then. This resulted in poorly controlled blood sugar levels. The patient was diagnosed with acute oro rhino orbital mucormycosis . rhino cerebral mucormycosis is the most common form of this fungus that occurs in people with uncontrolled diabetes ( https://www.cdc.gov/fungal/diseases/mucormycosis/definition.html ) the fungus enters the sinuses from the environment and then the brain.
The patient was also diagnosed with acute infarct in the left frontal and temporal lobe. Mucormycosis is associated with the occurrence of CVA ( https://journal.chestnet.org/article/S0012-3692(19)33482-8/fulltext#:~:text=There%20are%20few%20incidences%20reported,to%20better%20morbidity%2Fmortality%20outcomes. )
QUESTION: What is the efficacy of drugs used along with other non-pharmacological treatment modalities and how would you approach this patient as a treating physician?
The proposed management of the patient was –
1. inj. Liposomal amphotericin B according to creatinine clearance
2. 200mg Iitraconazole was given as it was the only available drug which was adjusted to his creatinine clearance
3. Deoxycholate was the required drug which was unavailable
https://pubmed.ncbi.nlm.nih.gov/23729001/ this article talks about the efficacy and toxicity of different formulations of amphotericin B
along with the above mentioned treatment for the patient managing others symptoms is also done by-
I. Management of diabetic ketoacidosis –
(a) Fluid replacement- The fluids will replace those lost through excessive urination, as well as help dilute the excess sugar in blood.
(b) Electrolyte replacement-The absence of insulin can lower the level of several electrolytes in blood. Patient will receive electrolytes through a vein to help keep the heart, muscles and nerve cells functioning normally.
(c) Insulin therapy- Insulin reverses the processes that cause diabetic ketoacidosis. In addition to fluids and electrolytes, patient will receive insulin therapy
QUESTION: What are the postulated reasons for a sudden apparent rise in the incidence of mucormycosis in India at this point of time?
Mucormycosis is may be being triggered by the use of steroids, a life-saving treatment for severe and critically ill Covid-19 patients. Steroids reduce inflammation in the lungs for Covid-19 and appear to help stop some of the damage that can happen when the body's immune system goes into overdrive to fight off coronavirus. But they also reduce immunity and push up blood sugar levels in both diabetics and non-diabetic Covid-19 patients.
With the COVID-19 cases rising in India the rate of occurrence of mucormycosis in these patients is increasing
9)Infectious Disease (Covid 19)
As these patients are currently taking up more than 50% of our time we decided to make a separate log link here:
http://medicinedepartment.blogspot.com/2021/05/covid-case-report-logs-from-may-2021.html?m=1
4)Covid 19 Mild
Link to the case report log:
4 Questions:
1. Is the elevated esr due to covid related inflammation?
Erythrocyte sedimentation rate (ESR) is a blood test. It measures how quickly erythrocytes, or red blood cells, separate from a blood sample that has been treated so the blood will not clot.
The sustained high level of ESR possibly brings a negative effect on COVID-19 patients' prognosis
However the elevation in esr cannot be explained based on the present knowledge on Covid
2. What was the reason for this patient's admission with mild covid? What are the challenges in home isolation and harms of hospitalization?
after 14 days of isolation he got tested again for COVID-19 which was positive . He then developed fever since 4 days, cough which was productive since 4 days and shortness of breath grade 3 since 2 days. He also had fatigue.He lost the sense of taste and smell.
Since the patient has SOB of grade 3. This poses a challenge for home isolation.
Patients with COVID-19 had almost 19 times the risk for acute respiratory distress syndrome (ARDS) than did patients with influenza, (adjusted risk ratio [aRR] = 18.60; 95% confidence interval [CI] = 12.40–28.00), and more than twice the risk for myocarditis (2.56; 1.17–5.59), deep vein thrombosis (2.81; 2.04–3.87), pulmonary embolism (2.10; 1.53–2.89), intracranial hemorrhage (2.85; 1.35–6.03), acute hepatitis/liver failure (3.13; 1.92–5.10), bacteremia (2.46; 1.91–3.18), and pressure ulcers (2.65; 2.14–3.27). The risks for exacerbations of asthma (0.27; 0.16–0.44) and chronic obstructive pulmonary disease (COPD) (0.37; 0.32–0.42) were lower among patients with COVID-19 than among those with influenza. The percentage of COVID-19 patients who died while hospitalized (21.0%) was more than five times that of influenza patients (3.8%), and the duration of hospitalization was almost three times longer for COVID-19 patients.
5)Covid 19 and comorbidity (Altered sensorium, azotemia, hypokalemia)
Link to the case report log:
5 Questions:
1) What was the reason for coma in this patient?
The patient has an spo2 of 20%. This might have lead to cerebral hypoxia thus leading to coma.
Also, low blood potassium can make you short of breath, as it can cause the heart to beat abnormally. This means less blood is pumped from your heart to the rest of your body
Thus low spo2 and thus coma
2) What were the competency gaps in hospital 1 Team to manage this intubated comatose patient that he had to be sent to hospital 2? Why and how did hospital 2 make a diagnosis of hypokalemic periodic paralysis? Was the coma related?
Hospital 1 might not have correlated Severe weakness of 4 limbs with low values of potassium which hospital 2 has diagnosed.
Yes, coma is related to Hypokalemia periodic paralysis as it might have caused cerebral hypoxia.
3) How may covid 19 cause coma?
After cessation of sedatives, the described cases all showed a prolonged comatose state.
unconsciousness after prolonged periods of mechanical ventilation in the ICU.
6 )SevereCovid 19 with altered sensorium
Link to the case report log:
6 Question
1. What was the cause of his altered sensorium?
Can be any of the following reasons
An altered state is any mental state(s), induced by various physiological( increased hospital stay) , psychological( mental depression due to isolation), or pharmacological maneuvers or agents( drugs of COVID)
2. What was the cause of death in this patient?
This patient is an elderly chronic alcoholic and smoker.
This might have delayed his healing process thus causing death
Also he had elevation LFT and RFT values
8)Covid 19 Moderate
Link to the complete case report log
8 Questions:
1. Can psoriasis be a risk factor for severe form of COVID?
Elderly psoriasis patients and/or patients using conventional immunosuppressive regimens and biologic agents are at higher risk for infectious diseases.
But the frequency of COVID-19 does not increase in patients using immunosuppressants, including those receiving biological therapy with a diagnosis of psoriasis
2. Can the increased use of immunomodulatory therapies cause further complications in the survivors?
According to the present knowledge on Covid,there is no indication that people taking immunomodulatory drugs for other diagnosed conditions should be concerned that their medication increases their risk for severe COVID-19,"
3. Is mechanical ventilation a risk factor for worsened fibroproliferative response in COVID survivors?
patients of Covid with greater fibrotic changes required more prolonged mechanical ventilation, and this in turn was associated with an increased severity of systemic organ failure.
Hence Mechanical ventilation is risk factor
11 )Covidmoderate with first time detected diabetes:
Link to Case report log :
Questions:
1) How is the diabetes related to the prognosis of COVID patients? What are the factors precipitating diabetes in a patient developing both covid as well as Diabetes for the first time?
Hypertension and severe obesity are common comorbidities in patients with diabetes. It is unclear whether diabetes alone contributes to increased risk of morbidity and mortality related to COVID-19. have indicated that poorer glycemic control is associated with poorer outcomes in people with diabetes
mechanisms that may increase the ability of COVID-19 to impact patients with diabetes:
higher affinity cellular binding and efficient virus entry; decreased viral clearance; diminished T-cell function; increased susceptibility to hyperinflammation and cytokine storm; and the presence of cardiovascular disease
pathogenetic link between diabetes and COVID-19. Both disease conditions involve inflammation with the release of inflammatory markers. The roles of angiotensin-converting enzyme molecule and dipeptidyl peptidase were explored to show their involvement in COVID-19 and diabetes. Pathogenetic mechanisms such as impaired immunity, microangiopathy, and glycemic variability may explain the effect of diabetes on recovery of COVID-19 patients. The effect of glucocorticoids and catecholamines, invasion of the pancreatic islet cells, drugs used in the treatment of COVID-19, and the lockdown policy may impact negatively on glycemic control of diabetic patients.
Patients with diabetes mellitus have increased predisposition to viral and bacterial infections including those affecting the respiratory tract
One of the mechanisms responsible for this predisposition is the “lazy” leukocyte syndrome, which represents impaired leukocyte function of phagocytosis (impaired immunity). This further emphasizes the likelihood of increased propensity of SARS-CoV-2 infections in diabetic cohorts
Microangiopathy in diabetes mellitus also impairs the lung compliance with consequent affectation of the gaseous exchange. This impairment may result in the proliferation of some respiratory pathogens including SARS-CoV-2
There are respiratory changes in diabetic patients that affect lung volumes and pulmonary diffusing capacity
Glycemic variability is a prognostic factor in diabetic patients with COVID-19 infection. Hyperglycemia worsens the outcome by the process of cytokine storm, endothelial dysfunction, and multiple organ injuries
In the lungs, the primary target of COVID-19, hyperglycemia leads to a rapid deterioration in spirometric functions, especially decreased forced expiratory volume in 1 second and forced vital capacity
hyperglycemic states, there is elevated glucose concentration in the respiratory epithelium which may affect its innate immune capacity. Hypoglycemia also increases cardiovascular mortality by accentuating monocytes which are pro-inflammatory and enhancing platelet aggregation
Severe hypoglycemia which may occur with strict glycemic control may worsen the overall mortality rate
suboptimal glycemic control in COVID-19 patients is correlated with higher mortality rate
Effect of COVID-19 on Diabetes:
COVID-19 infection compounds the stress of diabetes mellitus by releasing glucocorticoids and catecholamines into circulation. These worsen glycemic control and increase the formation of glycation end products in many organs and worsen prognosis
The degree of inflammatory response to COVID-19 is more marked in diabetic patients than in nondiabetic cohorts
showed that type 2 diabetic group had higher levels of inflammatory markers such as C-reactive protein and procalcitonin (57.0 and 33.3%) than the nondiabetic group (42.4 and 20.3%), respectively. Elevated C-reactive protein may serve as a marker for identifying those with high risk of death from COVID-19
D-dimer which is a marker of coagulation status was also elevated in the diabetic group compared to the nondiabetic group
The levels of these inflammatory markers have been correlated with the severity of COVID-19 infection
2) Why couldn't the treating team start her on oral hypoglycemics earlier?
To control the high range diabetes she is on insulin’s injections which have faster and effective action to control diabetes than oral hypoglycaemic drugs.
Insulin exhibits inhibitory action on ADAM-17 [35]. ADAM-17 enhances the proteolytic shedding of the enzymatic active ecto-domain of ACE2. This may suggest that insulin increases the activity of ACE2 [35] and also increases the infectivity of SARS-CoV-2
The beneficial effect of insulin may be related to its anti-inflammatory effect, which is by suppression of pro-inflammatory cytokines and increased immune mediators
Insulin use has effective glycemic control.which benefits a better prognostic results.
12) Moderate to severe covid with prolonged hospital stay:
Questions :-
1) What are the potential bioclinical markers in this patient that may have predicted the prolonged course of her illness?
The potential biochemical markers in this patient are
Elevated levels of
LFT- Total bilirubin : 1.24 mg/dl
Direct bilirubin : 0.67 mg/dl
SGOT : 73 units/ lit
SGPT : 80 units/ lit
ALP : 342 units/ lit
RFT Blood urea : 34 mg/dl
Sodium : 150 meq/lit
Potassium : 5.2 meq/lit
SERUM LDH 571 units/lit
FBS 332 mg /dl
13)) Severe covid with first diabetes
Link to Case report log :
What are the consequences of uncontrolled hyperglycemia in covid patients?
Answer:
•Severe inflammatory changes in lungs in case of covid pneumonia.
•Delayed recovery of the patient .
Since elevated blood sugar levels favors the virus growth and multiplication.
Does the significant rise in LDH suggests multiple organ failure?
Answer:
High LDH levels
Extremely high levels of LDH could indicate severe disease or multiple organ failure. Because LDH is in so many tissues throughout the body, LDH levels alone won't be enough to determine the location and cause of tissue damage.
What is the cause of death in this case?
Answer:
Cause of death could be most probably due to:
•Severe covid pneumonia associated with uncontrolled hyperglycaemia
•Multiple organ failure
18)Covid 19 with mild hypoalbuminemia
Question 1:
What is the reason for hypoalbuminemia in the patient?
Answer:
It may be due to pulmonary capillary leakage in lungs , in response to epithelial endothelial damage due to covid infection.
https://pubmed.ncbi.nlm.nih.gov/33411411/2.
Question 2:
What could be the reason for exanthem on arms? Could it be due to covid-19 infection ?
Answer:
Yes, what the patient is experiencing is known as viral exanthem which is one of the cutaneous manifestation of COVID-19.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7549735/
Question 3:
What is the reason for Cardiomegaly?
Answer:
The most probable cause of that appearance is AP view of the chest. When an anteroposterior view is taken, most times the CXR shows false cardiomegaly. To confirm the cardiomegaly a PA view of chest must be taken.
Another possible cause can be Direct Myocardial Cell Injury. The interaction of SARS-CoV-2 with ACE2 can cause changes to the ACE2 pathways, leading to acute injury of the lung, heart, and endothelial cells. A small number of case reports have indicated that SARS-CoV2 might directly infect the myocardium, causing viral myocarditis. However, in most cases, myocardial damage appeared to be caused by increased cardiometabolic demand associated with the systemic infection and ongoing hypoxia caused by severe pneumonia or ARDS
https://www.ncbi.nlm.nih.gov/books/NBK556152/
Question 4:
What other differential diagnoses could be drawn if the patient tested negative for covid infection?
Answer:
Possible alternative diagnoses may include:
• Influenza
• Mycoplasma pneumonia
• Parainfluenza
• Respiratory syncytial virus
• Streptococcus pneumonia
• Other viral or bacterial pneumonia.
Question 5:
Why is there elevated D-Dimer in covid infection? What other conditions show D-dimer elevation?
Answer:
It is well known that D-dimer are produced during fibrin breakdown and serve as a marker of fibrinolytic activity. A relationship between proinflammatory cytokines and markers of activation of the coagulation cascade, including D-dimer, has been demonstrated in critical patients or patients with sepsis .There is also evidence that under inflammatory conditions, the alveolar haemostatic balance is shifted towards a predominance of prothrombotic activity .In addition, pro-inflammatory cytokines may be involved in endothelial injury, and may activate coagulation and inhibit fibrinolysis in patients with severe sepsis.
• D-dimer can be elevated such as in pregnancy, inflammation, malignancy, trauma, liver disease (decreased clearance), heart disease, sepsis or as a result of hemodialysis, CPR or recent surgery)





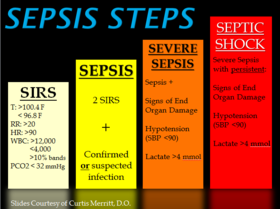
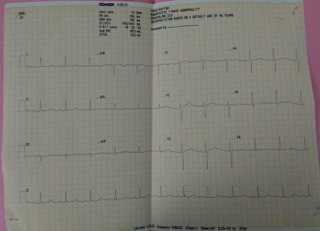
Comments
Post a Comment